Michael Webberley - Analysis of Androgen Patients & Androgen Practice
Analysis of Determination on the Facts
The determination on the facts in the Medical Practice Tribunal Service (MPTS) case against Dr. Michael Webberley (MW) ran to 305 typed pages. It was publicly available from the MPTS for a short period of time; a copy can be viewed here: Full text of MPTS Determination on the Facts. Dr Webberley was erased from the medical register based on the outcome of the tribunal.
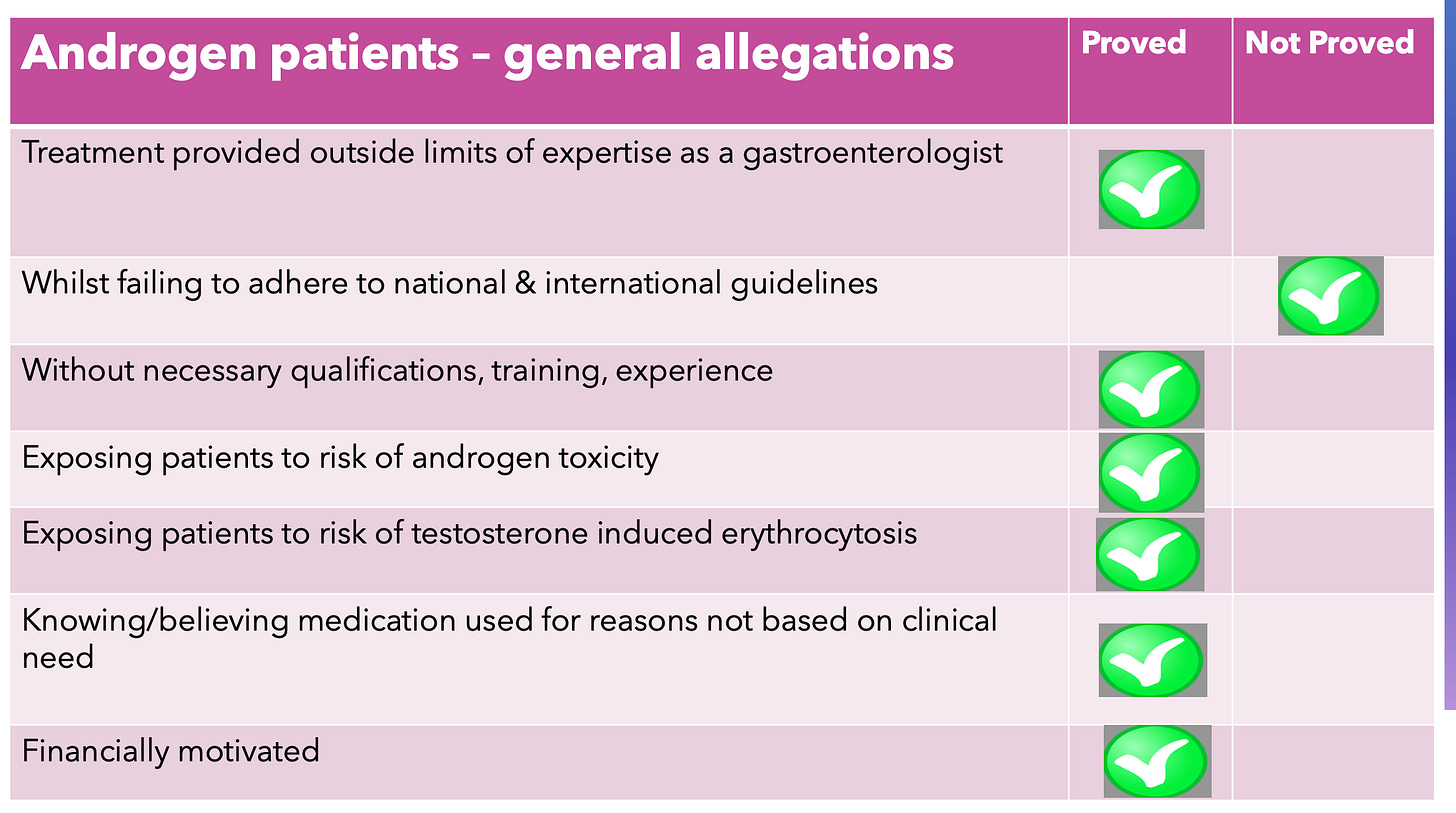
There are four broad categories of allegations against MW:
general failures of care in treatment of the 18 patients referred to as androgen patients (7 allegations, 6 allegations proved);
specific and detailed failures in the provision of good care to 18 patients with regard to androgen therapy (441 specific allegations, 259 allegations proved);
specific and detailed failures in the provision of good care to 7 patients with regard to transgender therapy; and
general failures in running an online clinic ‘Gender GP’.
This document is an analysis of the determination of the facts on the first two categories of allegations above; those relating to the androgen patients. The MPTS document is difficult to use. The detailed allegations are repeated 3 times in the document. Not all allegations apply to all patients. There are allegations that appear to be the same in substance (based on detailed discussion in the document) but have use a different form of words.
Press reports have quoted ‘25 patients, 89 allegations’. The 25 patients can be reconciled - identified by the MPTS as Patients A - Y). The MPTS grouped multiple individual allegations together in a non-standard manner. For purposes of the analysis - each individual specific allegation that could be proved or not proved is counted as a separate allegation.
The allegations and the analysis of the MPTS are highlighted with excerpts from the determination of facts. This analysis was under taken by members of the Tribunal Tweets volunteer collective, who attended the tribunal in person and reported daily on the hearings. See our coverage of MW’s tribunal here.
General allegations: 7 alleged, 6 proved
The general allegations are introduced in the MPTS Determination of Fact at paragraphs 63 a&b. The analysis of the allegations is paragraphs 501 to 512. Selected quotes:
Para 503…… the Tribunal concluded that Dr Webberley was under a duty not to work outside the limits of his expertise, or without the necessary qualifications and training in the field in which he was purporting to practice. ……However, the Tribunal did not have any evidence that Dr Webberley had undergone training or qualification in endocrinology, particularly in relation to hormone deficiency syndromes.
Para 509 The Tribunal was wholly satisfied that in numerous respects the treatment provided by Dr Webberley to Patients A to R was not in accordance with recognised medical practice for the treatment of male hypogonadism. The Tribunal, in these circumstances, suspected that the treatment provided to these patients did not adhere to national and international guidelines current at the relevant time. Indeed, Dr Quinton asserted in his report that, in his opinion, Dr Webberley had failed to treat patients in accordance with national and international guidelines. However, the Tribunal noted that the only guidelines to which Dr Quinton had made specific reference were those referenced above, and which were published in 2021. Therefore, they could not have been guidelines Dr Webberley would have been required to adhere to in respect of these patients. For this reason, and for this reason alone, the Tribunal found paragraph 63aii of the Allegation not proved.
Para 511….the Tribunal determined that Dr Webberley’s misdiagnosis of, and treatment for, male hypogonadism in respect of Patients A to R, was not simply as a result of incompetence borne of a lack of expertise, qualification, training and or experience. Rather, it was done knowing or believing that the treatment was neither clinically indicated nor necessary……… Furthermore, on numerous occasions, not only was Dr Webberley prescribing treatment regimens that had no recognised medical application for the treatment of hypogonadism, and which were characteristic of those sought by ‘body builders’, the patients themselves were invariably indicating a desire or preference to be prescribed these treatment regimens before Dr Webberley had made any diagnosis. In the Tribunal’s judgement, Dr Webberley’s conduct in this regard was entirely consistent with his knowing or believing that his patients were seeking the prescriptions for reasons other than clinical need.
Androgen Patients - Specific Allegations - 441 alleged, 259 proved
There were 18 androgen patients considered by the tribunal, referred to as Patients A-R. Many allegations were repeated across multiple patients, but each patient was unique. The maximum number of specific allegations for a single patient was 35 for Patient L, of which 26 were proved. The minimum number was 13 for Patient R. None of those were proved - R was the only patient where all allegations were found ‘not proved’ against MW.
The allegations relating to Patient R were found ‘not proved’ against MW because
para 499…… considering the evidence overall, the Tribunal was not satisfied, on the balance of probabilities, that it was in fact Dr Webberley who was responsible for either the care of Patient R or the prescription of drugs to him.
Failure to consult with patient
Example allegation:
1. You failed to provide good clinical care to Patient in that you:
a. did not hold a consultation with Patient.
Excerpt from determination of facts:
Para 85 …Dr Quinton explained that a consultation was necessary for a number of reasons, not least of which is the need to ensure that the patient was seeking testosterone treatment for a bona fide medical condition, as opposed to, for the purpose of achieving other perceived benefits of testosterone, namely, a more ‘sculpted’ body, better muscle definition and sometimes a wish for improved sexual desire and performance. Dr Quinton’s evidence was that by ‘eyeballing’ the patient it is sometimes immediately obvious that they are unlikely to be hypogonadal, for example, from their evidently muscular physique.
Failure to take and document an adequate history
Example allegations:
You failed to provide good clinical care to Patient in that you:
a. consulted with Patient and failed to:
i. elicit an adequate medical history in that you:
1. relied upon details obtained by a non-medically trained member of staff;
2. failed to elicit details of sexual symptoms;
3. failed to elicit details of non-sexual symptoms;
4. failed to ask general health questions concerning the presenting complaint;
Excerpt from determination of facts:
Para 89 …. the medical records demonstrated that the only medical history that Dr Webberley had was an online questionnaire with a series of tick boxes to enable the patient to indicate; ‘yes’ or ‘no’, to such matters as ‘health habits and personal safety’, ‘mental health’, the presence or absence of particular symptoms and ‘quality of life assessment’ coupled with the opportunity for the patient (if they so chose) to provide further detail in respect of those questions they had answered in the affirmative.Although Dr Quinton doubted the utility of this questionnaire, his criticism was not so much directed at the questions themselves, but rather, that Dr Webberley failed to ask directed follow up questions that ‘drilled down’ or expanded on relevant sexual features (reduced libido, erectile dysfunction, and loss of waking erection) and non-sexual features (anaemia, osteoporosis, gynecomastia and sweating and flushing), potentially related to hypogonadism. It could only be through further enquiry that the doctor would be able to form a proper clinical judgement as to the probable cause of the symptoms.
90. The Tribunal accepted that the medical history, limited as it was to the answers given in the online health questionnaire, was inadequate in that it failed to elicit details of sexual and non-sexual symptoms and the answers given to general health questions concerning the presenting complaint as identified by Dr Quinton.
Failure to perform any physical or mental health examination
Example allegation
‘Did not perform any physical or mental health examination of patient’
Excerpt from determination of fact
412. In the case of Patient N, unlike some of the other patients that the Tribunal considered, there was email correspondence between Patient N and Dr Webberley/GenderGP which demonstrated that Patient N was reporting a variety of different symptoms, both physical and mental health, and there had also been a number of blood tests. Furthermore, the Tribunal considered that there were indications within Patient N’s communications with Dr Webberley/GenderGP that he might be someone who was displaying androgen seeking behaviour. In particular, in the manner in which he sought to dictate to Dr Webberley how he wanted his testosterone.
413. In these circumstances the Tribunal determined that Dr Webberley should have conducted both a physical and mental health examination before prescribing.
Failure of diagnosis and diagnostic procedures
Example allegations:
‘inappropriately diagnosed Patient with hypogonadism in that:
i. the diagnosis was not supported by laboratory results;
ii.you failed to consider any alternative diagnosis;’
Excerpt from determination of fact
100. ……. the Tribunal accepted Dr Quinton’s opinion that, in the light of an absence of any evidence of hypogonadism, Dr Webberley should have considered a differential diagnosis, such as ‘androgen seeking behaviour’ against a background of significant mental health issues. This was particularly so as Dr Quinton had observed that, at the outset of the questionnaire, Patient had indicated that the type of treatment he was seeking was balanced TRT with hCG (Human Chorionic Gonadotropin) and oestrogen control (a treatment regime that Dr Quinton opined would be typically described as ‘stacking’). Also, from the answers given in Patient’s questionnaire there was evidence of symptoms and problems suggestive of a person who was vulnerable and who might have had mental health issues.
Prescribing that was unsafe, not clinically indicated, inappropriate dosage and other failures
Example allegations:
‘prescribed testosterone, Human Chorionic Gonadotropin (‘hCG’) and anastrozole which was:
i. not clinically indicated;
ii. unsafe;
iii.not recognised as therapeutic practice in medicine;
Excerpt from determination of fact
Para 104: ‘Dr Quinton’s evidence was that excessive doses of testosterone are associated with serious risks, these include erythrocytosis (increase in number of red blood cells), risks of a venous thrombo-embolism, myocardial infarction, stroke and growth of pre-existing prostate cancer amongst other things. Furthermore, in Dr Quinton’s opinion Patient A, who had pre-existing normal levels of testosterone, was being prescribed double the dose of testosterone that one would expect for a man with hypogonadism. In the Tribunal’s judgement, given the risks associated with excessive levels of testosterone, and the doses which Dr Webberley was prescribing Patient A, it was self-evidently both unsafe and unnecessary to do so.’
Testing; failure to test, failure to set appropriate conditions for tests and follow up tests
Example allegations:
Failed to provide good clinical care to Patient in that you:
f. did not conduct tests adequately in that you failed to check Patient’s full blood count;
g. did not identify that repeat blood tests were contrary to your diagnosis of hypogonadism;
Excerpt from determination of fact:
265. The laboratory test results within BMH’s patient record obtained both before and after prescription did not include full blood count tests (December 2017, March 2018 x2 and April 2018), which they should have done, particularly once testosterone had been prescribed.
267. The Tribunal determined that Dr Webberley, obtained the results of two separate blood tests both received during December 2017, the results of which were both contrary to a diagnosis of hypogonadism. Nevertheless, in January 2018, Dr Webberley again prescribed testosterone cream for the treatment of hypogonadism.
Failures in communication; not responding to patient concerns, not supervising non-medical staff, not providing specific instructions
Example allegations:
did not adequately communicate with Patient;
did not provide adequate follow up care in that you:
ii.delegated communications with Patient to non-medically trained members of staff.
Excerpt from determination of fact:
269. The Tribunal found these allegations proved. The Tribunal acknowledged that BMH records showed some limited email communication as between Dr Webberley and Patient G. However, in the main, it appeared that Patient G was communicating with non-medically trained members of staff. In particular, the Tribunal noted that on 12 March 2018 a complaint by Patient G was recorded in the following terms:
“contacted doctor with urgent symptoms via direct email and didn’t get a response at all “does Dr Webberley really exist”.
270. On 13 March 2018, the following day, Dr Webberley responded to a member of BMH staff as follows:
“emailed me, anxiety +++… just for the record I went through all this with him in January too… so the doctor does exist”.
271.The Tribunal determined that given Dr Webberley had been made aware of his patients’ distress, his response was inadequate both in terms of communication and providing adequate follow up care.
Not providing adequate follow up care
Example allegation:
Failed to provide good clinical care to Patient in that you:
g. did not review Patient’s treatment plan;
h. did not adequately communicate with Patient;
i. did not provide adequate follow up care;
Excerpt from determination of fact
249. The Tribunal did not have sight of any medical records from BMH in relation to Patient F. However, Patient F’s evidence was that he emailed Dr Webberley as he had a number of questions concerning his treatment and, in particular, an enquiry concerning a recent review blood test that showed his testosterone to be over the upper end of the (normal) scale. He received no response from Dr Webberley and sent a further email, this time copied into one of the ‘facilitators’ (one of the non-medically trained members of staff). In response, Patient F received a telephone call from one of the facilitators who did answer his questions. At this stage Patient F was concerned at what appeared to be (BMH’s) ‘cavalier attitude’ towards medicine and so he went to an alternative medical provider (MHC).
250. The Tribunal considered that, at the very least, and accepting Dr Quinton’s evidence, Dr Webberley having been contacted by Patient F in relation to abnormal blood test results, should have reviewed the treatment plan, should have communicated with Patient F and provided follow up care, which he did not do.
Failure to review treatment plans or amend treatment plans on follow up testing
Example allegation:
Failed to provide good clinical care to Patient in that you:
f. did not review during treatment:
i. feedback from Patient regarding his treatment;
ii.Patient’s laboratory results.
Excerpt from determination of fact
372. The Tribunal, having considered Patient L’s medical notes in their entirety and, in particular, the chronological patient contact record, determined, on the balance of probabilities that, Dr Webberley had not reviewed Patient L’s treatment following either the feedback from Patient L regarding his treatment or his laboratory test results. The Tribunal determined, accepting Dr Quinton’s evidence, that he should have done both.
Did not maintain adequate records
Example allegation:
Failed to provide good clinical care to Patient in that you:
j. did not maintain adequate medical records throughout the period of treatment of Patient.
Excerpt from determination of fact
380. The Tribunal reminded itself that although Patient L had entered into an agreement with BMH, Patient L was the patient of Dr Webberley, and it was Dr Webberley who was responsible for Patient L’s clinical care in respect of which he should have maintained an adequate medical record. The Tribunal, having considered Patient L’s medical notes, found that they contained comprehensive records of interactions between BMH’s non-clinical staff and Patient L. However, there were minimal clinical records concerning Dr Webberley’s care of Patient L. They were limited to a note of the consultation on 8 March 2018 and an apparent endorsement by Dr Webberley of what appeared to be a treatment decision by Mr MK.
381. Further, although not necessary for the purpose of its determination in relation to this paragraph, the Tribunal noted that the records suggested that Dr Webberley apparently made a diagnosis and then prescribed testosterone on 21 February 2018, some two weeks before his initial consultation with Patient L on 8 March 2018.
Failure to properly obtain informed consent; including misleading information on consent forms and omission of risks
Example allegations
17. The Consent Forms provided to Patient stated that:
a. the higher limit of normal testosterone range was 40 nmol/L;
b. untreated hypogonadism can increase risk of:
i. heart disease;
ii. Alzheimer’s disease;
iii. premature death;
c. the treatment provided was TRT;
18. You knew that the information in the Consent Forms was untrue as:
a. 40 nmol/L exceeded laboratory normal ranges for testosterone;
b. there was a lack of evidence that untreated hypogonadism increased the risk of:
i. heart disease;
ii. Alzheimer’s disease;
iii. premature death;
c. the treatment provided increased testosterone above normal limits and was not TRT;
Excerpt from determination of fact
127. The Tribunal had regard to the Participation Agreement & Informed Consent Form and the Consent for Testosterone Replacement Therapy Form, which detailed the above factual statements (‘the Consent Forms’) signed by Patient A on 29 June 2017.
128.Accordingly, the Tribunal found paragraphs 2a and bi, ii, iii and c of the Allegation proved.
130. The Tribunal concluded from the evidence before it that Dr Webberley must have been familiar with laboratory blood test results and the normal ranges quoted therein. Accordingly, the Tribunal determined that Dr Webberley must have known that the higher (upper) limit quoted in BMH’s consent form was untrue.
Dishonest conduct with individual patients
Example allegations
Your conduct as set out at paragraph x (documentation of consent) was dishonest by reason of paragraph Y (consent forms containing inaccurate or false statements)
Excerpt from determination of fact
141. The Tribunal, having determined that paragraphs 2a and 3a were proved, went on to consider whether Dr Webberley’s conduct was dishonest in this regard. The Tribunal determined that Dr Webberley, in using a consent form that he knew falsely stated the higher limit of normal testosterone to such an excessive degree was self-evidently dishonest and would be regarded as such by the standards of ordinary decent people.
142. In particular, the Tribunal considered that the only purpose which Dr Webberley could have had in knowingly making this untrue statement, would have been to either, in due course, mislead his patient into believing that he had a medical condition requiring treatment, namely hypogonadism and that TRT/TT was necessary or, alternatively to create the impression to others that he was providing treatment to Patient A for a bona fide medical condition as opposed to prescribing inappropriately for the purpose of, for example, ‘body sculpting’ or enhanced athletic performance.
143. In reaching this conclusion, the Tribunal considered it significant that within the consent form not only was the upper limit of normal testosterone range inflated, it was also stated that to obtain the full benefits of testosterone, the purpose of the therapy was to restore testosterone levels to the ‘optimal’ range and not the ‘normal for age’ range. This specifically meant potentially raising the patient’s testosterone level to the higher (upper) quarter of the untruthful reference range, stated to be 24/40 nmol/L.
Documentation of informed consent
Example allegations
You did not obtain informed consent from Patient for treatment you provided in that:
a. you failed to counter-sign the Consent Forms;
b. the Consent Forms contained statements which were untrue.
Excerpt from determination of fact
146. The Tribunal, having concluded that the consent form provided untruthful information, both in relation to the risks associated with untreated hypogonadism, and as to the normal higher (upper) limits of testosterone, determined that Patient A could not have provided informed consent on the basis of the contents of this document. Rather, any consent obtained would have been misinformed.